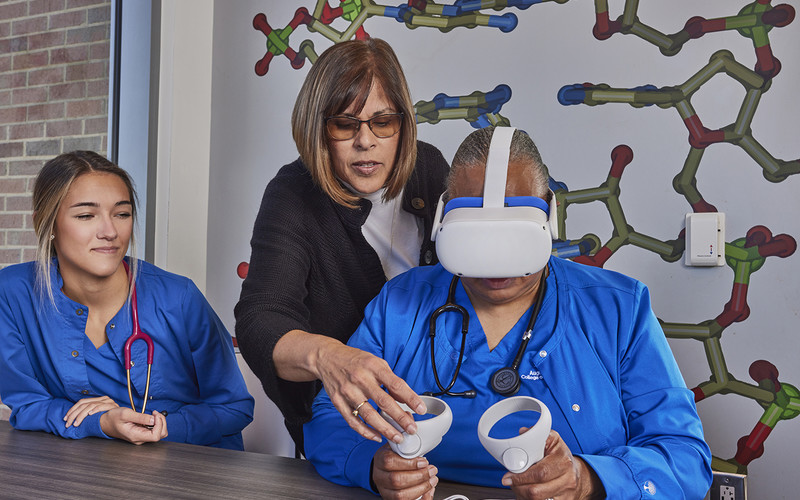
With VR headsets, computers and software, students can dissect virtual cadavers; train for surgery, intubation and other procedures; and practice medical situations, from examining and diagnosing patients to handling hospice care.
“There’s tremendous value in being able to replicate real-life scenarios and try things again and again,” says Bob O’Donnell, founder and chief analyst at TECHnalysis Research. “Doing virtual surgeries — and in the case of virtual cadavers, letting people peel away the layers and explore the body — helps people figure out how everything works.”
According to the National Library of Medicine, educators can use different forms of VR in a medical school environment, including 360-degree video and interactive VR. The technology also offers cost savings compared with physical simulations, with the main upfront costs being the hardware and software.
The technology requires less space than physical simulations and can free up faculty time because, in some cases, instructors do not need to be present, the National Library of Medicine notes.
READ MORE: How virtual reality advances bring new possibilities to higher education.
Augusta University Nursing Students Practice End-of-Life Situations
At Augusta University, two nursing professors collaborated with the university’s Center for Instructional Innovation to create six immersive, end-of-life VR scenes that students can view on an Oculus VR headset.
The scenes, each lasting one to three minutes, include telling family members that their loved one is near death and explaining why the patient looks and sounds the way they do. In another scene, an anguished family member asks if she can bring her 4-year-old child into the room to say goodbye.
To build the VR scenes, they first wrote scripts, then filmed the scenes using a 360-degree video camera and microphones, using students and staff as actors inside a patient room at the university’s healthcare simulation center.
During production, they painted visual effects on the patient’s skin and added vocal audio effects to replicate what patients look and sound like at the end of life, Steinberg says.